Playlist
Show Playlist
Hide Playlist
Response-to-Injury Hypothesis
-
Slides Pathogenesis of Plaque Formation.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
00:00
We've been discussing
risk factors and kind of the
general features of atherosclerosis.
00:06
Let's get a little bit
down into the details
about how the plaque
actually forms
because this also informs our
thinking about how we can maybe
inhibit that process and maybe
even reverse the process.
00:21
So we're talking
about pathogenesis.
00:24
Here we are,
roughly halfway through the
roadmap for atherosclerosis.
00:31
Again, by way of a review,
remember that atherosclerosis
is an interval based process.
00:38
It's composed of
dysfunctional endothelial,
a fibrous cap,
overlying and atheromatous core
and driven by macrophage and other
inflammatory cells and processes.
00:54
That leads to
narrowing of vessels
or to destruction
of the vessel wall.
00:59
Pretty straightforward.
01:01
Let's go now into
greater detail.
01:04
How does this happen?
And beginning in about the 60s,
early 70s, we thought what was going on
is that endothelium was damaged
and that all of atherosclerosis
was response to injury.
01:17
So that hypothesis, were showing a
vessel cross section of the wall,
the lavender cells
on top endothelium,
the orange cells in
the middle media.
01:26
And we thought there was an
injury to the endothelium,
we would erode or
denude the endothelium.
01:34
Platelets would bind,
because we've exposed the
underlying extracellular matrix.
01:40
We would then get the production
of pro-inflammatory,
pro-growth factors
made by those
activated platelets.
01:49
And we would do that over
and over and over again.
01:53
And that would give
us atherosclerosis.
01:57
Pretty straightforward.
01:58
A brilliant hypothesis,
except it wasn't
really accurate.
02:03
It turns out,
because in this hypothesis,
endothelial loss,
denudation was a key feature,
that turned out to
be what was wrong.
02:12
And in fact,
the endothelium is not
lost in atherosclerosis.
02:17
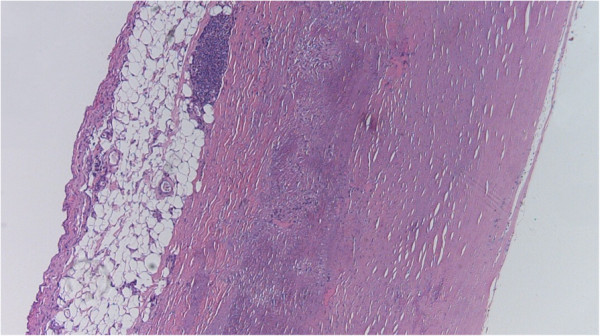
So this is a transmission
electron micrograph
of a vessel wall,
and the cell labelled at
the top is endothelium.
02:26
The cell with the kind of the
cleared areas is a macrophage.
02:29
And the underlying kind of white
stripe is the internal elastic lamina.
02:38
And in this,
in the internal elastic
lamina allows us to demarcate
everything above that is
going to be the intima,
everything below that is
going to be the media.
02:47
And the macrophage
is already there.
02:48
Remember, macrophages are going
to be a major driving force,
a pro-inflammatory
innate immune response,
that's going to be
driving atherosclerosis,
the macrophages
already in the intima.
03:00
And yet the endothelium
is perfectly fine.
03:04
It's still there.
03:05
So we never lose the
endothelium and atherosclerosis
in the typical way that
atherosclerosis develops.
03:15
This gets back to thinking about
the normal health and maintenance,
the care and feeding of
your endothelial cells,
and normal tension, normal blood
pressure, normal laminar flow,
normal growth factor
production by under line cells
and epithelial cells,
fibroblasts, macrophages,
normal cytokine production
and normal levels of oxygen NPH
lead to a healthy state
of the endothelium.
03:44
And that endothelial will make
appropriate levels of growth factors
and vasoactive mediators
controlling whether the
vessel tone is increased,
or, relaxed,
it will make appropriate
levels of adhesion molecules
and anticoagulant so that
blood stays in a liquid phase.
04:02
So a healthy happy
endothelial cell
actually requires the input of
a number of normal conditions
to have normal outputs.
04:11
Let's talk about
endothelial dysfunction.
04:14
So when we have turbulent flow,
when we have hypertension,
when we have increased
inflammatory cytokines,
when we have
activated compliment,
bacterial products,
cholesterol and
other lipid products,
if we have advanced glycation end
products as associated with diabetes,
if we have too high
level of hypoxia,
or acid,
if we have other inflammatory things
like viruses and cigarette, smoke,
we have endothelial
cell dysfunction.
04:45
And now the endothelial
cells make abnormal levels
and different suites of
growth factors and chemokines
to recruit inflammatory cells,
they make other cytokines,
they are more pro-coagulant,
they're going to be
more likely to clot.
05:00
They're going to be more
likely to be adhesives.
05:03
So to recruit
inflammatory cells,
they're going to make
more vasoactive mediators
so that we're going to
tend to see vasospasm.
05:11
And we're going to see increased
levels of histocompatibility molecules
so that we have an increased
inflammatory response.
05:19
So endothelial dysfunction
not endothelial loss
is what is going to be
the primary initial driver
for the development
of atherosclerosis.
05:29
Just as an example of that,
if we look on this,
on this image, control blood vessel
that is not inflamed and not activated.
05:40
Labelled inflammatory cells,
in this case,
neutrophils that have a fluorescent label
built into them,
do not stick to the vessel wall.
05:49
If we stimulate on
the right hand side,
those same blood vessels with
various inflammatory cytokines,
interleukin1 tumour
necrosis factor,
or other things such as
certain cholesterol byproducts,
we will now activate
that endothelium.
06:05
It will become dysfunctional
and will suddenly recruit a
whole bunch of neutrophils,
which will release their
inflammatory mediators
and will begin to drive the process
of atherosclerosis development.
06:15
So, endothelial
activation and dysfunction
very much are the
upstream drivers
of atherosclerosis development.
About the Lecture
The lecture Response-to-Injury Hypothesis by Richard Mitchell, MD, PhD is from the course Atherosclerosis.
Included Quiz Questions
The primary cause of atherosclerotic plaque formation is...
- ...endothelial dysfunction.
- ...increased pro-inflammatory substances.
- ...endothelial loss.
- ...endothelial hyperplasia.
- ...chronic cell injury.
What is the normal flow in a blood vessel?
- Laminar flow
- Rotational flow
- Turbulent flow
- Unsteady flow
- Compressible flow
How does a dysfunctional endothelium stimulate plaque formation?
- Increases cytokines
- Prevents hypoxia
- Controls acidosis
- Maintains normotension
- Regulates growth factors
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |